The way we view the prevention, diagnosis, and treatment of neurocognitive diseases like Alzheimer’s disease and other causes of dementia is continuously evolving, promoting a shift from a reactive to a proactive preventive approach in healthcare. While much of the research surrounding dementia has been focused on potential treatments and therapies, a significant amount of research has been dedicated to understanding the pathogenesis of disease development.
Research has revealed there is a connection between mood disorders like depression and the development and progression of dementia, giving rise to promising methods to prevent and even treat dementia. However, people can often become confused about this connection and what it means for them. Some people living with depression are worried they will inevitably develop dementia and are asking their doctors if depression can be a precursor to dementia.
To clear up any confusion, let’s take a look at the connection between depression and dementia, the risk factors involved in the development and progression of dementia, and the importance of early neurocognitive testing for those with mental health issues.
It’s important to note that depression does not directly cause dementia—rather, depression may contribute to other risk factors known to increase the risk of developing dementia. In other words, depression can be a precursor to dementia, but not in the way you may think. It appears that depression and its associated lifestyle impacts may be a modifiable risk factor for Alzheimer’s disease and other causes of dementia.
Research studies continue to demonstrate the significant association between depression symptoms and dementia. One study suggests that depression symptoms before the onset of Alzheimer’s disease are associated with the pathogenesis of Alzheimer’s, even when the first depression symptoms occurred more than 25 years before the onset of Alzheimer’s. This indicates that depression symptoms are a risk factor for the future development of Alzheimer’s.
There is a clear link between depression and dementia, but the main connection lies between the symptoms of depression and dementia. Depression symptoms, such as social isolation and lack of stimulation, have been recognized as modifiable risk factors for dementia.
Social isolation, social withdrawal, and lack of mental and social stimulation are common lifestyle impacts that often accompany depression.
Several studies suggest that maintaining social and mental activity throughout life may support brain health and decrease the risk of developing dementia. Meta-analyses found that social isolation or loneliness in older adults is associated with a 50% increased risk of developing dementia.
In addition to the evidence of this connection in research, emerging theories suggest that social and neurocognitive stimulation can help build up your “cognitive reserve,” where cognitive reserve refers to your brain’s ability to efficiently use networks of neuron-to-neuron connections. This enables individuals to effectively execute neurocognitive tasks, even as the brain changes over time.
The pathology of dementia is complex. Many causes of dementia are multifactorial, meaning they are not caused by a single factor, but rather develop from some combination of several factors, such as genetics, environment, and lifestyle.
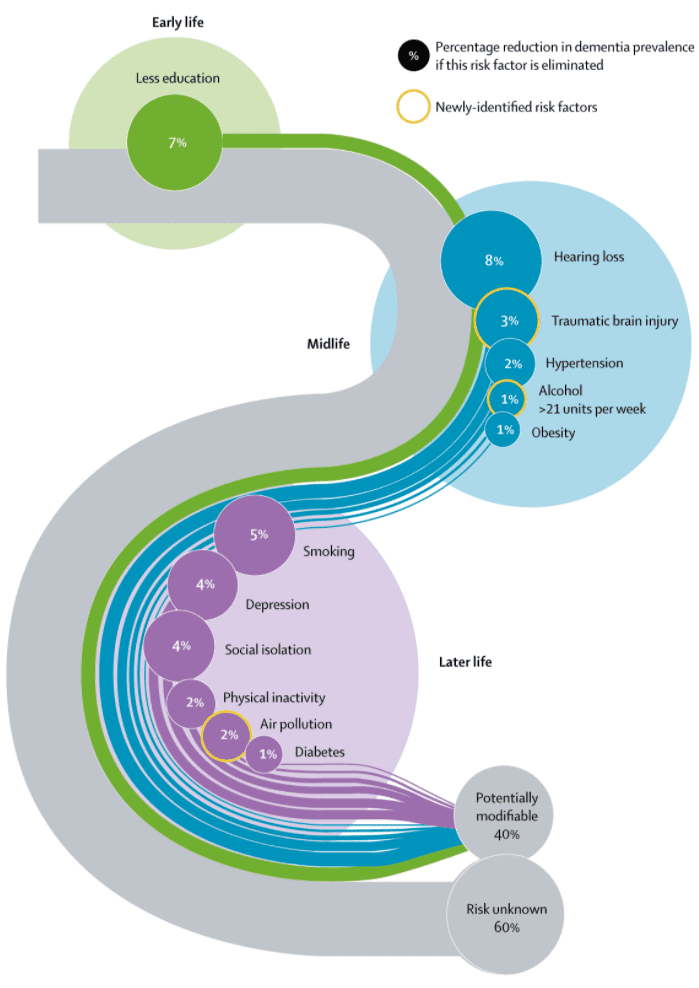
The Lancet Commission on Dementia prevention, intervention, and care identified 12 potentially modifiable risk factors that account for approximately 40% of worldwide dementias.
|
Stage of Life |
Modifiable Risk Factor for Dementia (% of dementia prevalence if this risk factor is eliminated) |
|
Early Life |
|
|
Midlife |
|
|
Later Life |
|
Like many other diseases and disorders, early intervention and early treatment are likely to produce better health outcomes. Early testing and monitoring of neurocognitive brain health are critical for the early identification of impairment and early intervention for all individuals, but particularly for those with risk factors like depression and other mental health issues.
It is never too early to understand and monitor your brain health. It is a vital part of overall wellness and plays a key role in our ability to live long, healthy, and full lives.
Altoida’s mission is to accelerate and improve drug development, neurological disease research, and patient care. To learn more about our precision-neurology platform and app-based medical device, contact us!