Lewy body dementia, or dementia with Lewy bodies, is believed to be the third most common cause of dementia after Alzheimer’s disease and vascular dementia, accounting for approximately 5% to 10% of dementia cases. However, the pathology of Lewy body dementia and its risk factors are far less established and understood when compared to other causes of dementia, such as Alzheimer’s disease.
Below, we provide information on established and potential risk factors for Lewy body dementia and how to monitor the brain health of individuals at risk of developing Lewy body dementia.
Lewy body dementia is a cause of progressive dementia that is clinically characterized by a decline in thinking, reasoning, and independent function. Symptoms include visual hallucinations, changes in cognitive abilities (thinking, reasoning, memory, and attention), changes in movement and gait, sleep disturbances, malfunctions of the autonomic nervous system, and depression.
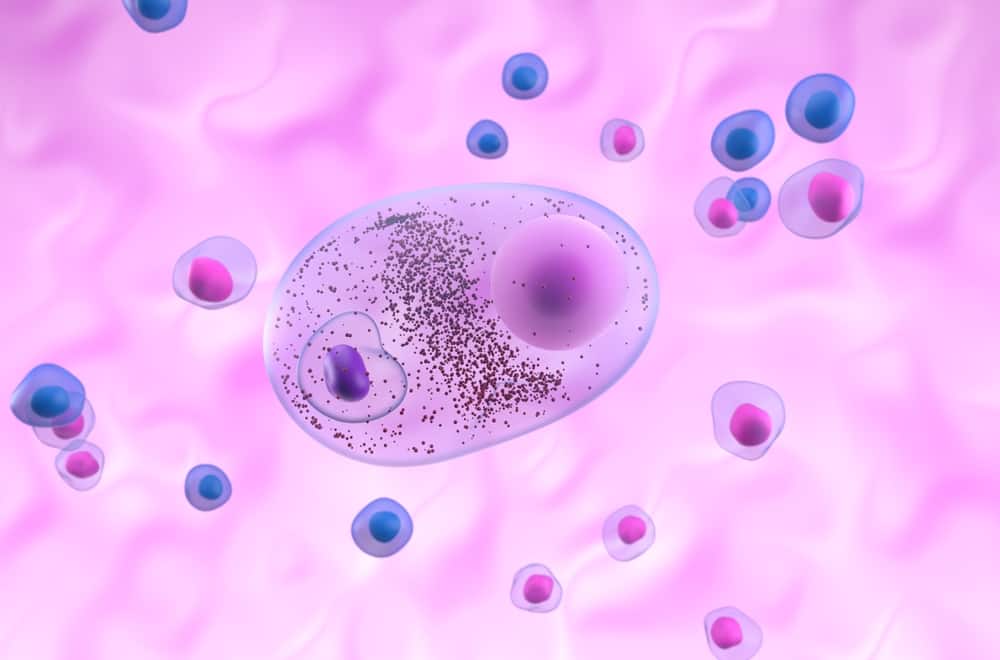
Neuropathological hallmarks, or key characteristics, of Lewy body dementia include the deposition of Lewy bodies and Lewy neurites. Lewy bodies, protein deposits made of abnormal filaments composed of alpha-synuclein, develop in nerve cells (neurons) within the regions of the brain responsible for memory, thinking, and motor control. Alpha-synuclein is found naturally in the brain; however, its function is not yet fully understood. Lewy neurites are abnormal neurites in diseased neurons and contain granular material and abnormal alpha-synuclein filaments similar to those in Lewy bodies.
Although Lewy body dementia risk factors are less established and less understood than risk factors for other neurodegenerative diseases, several potential risk factors have been identified. Established and generally agreed-upon risk factors for Lewy body dementia include age, family history, and sex, described in more detail below.
Conditions linked to vascular problems, such as hypertension, hyperlipidemia, and diabetes mellitus, as well as conditions that may result in social isolation and a lack of brain stimulation, like depression and loneliness, have been linked to many neurodegenerative and neurological diseases and conditions. Research suggests these conditions may also be risk factors for Lewy body dementia.
While there are no proven strategies for preventing Lewy body dementia, several aspects of healthy living may reduce the risk of developing dementia. In general, what is good for your heart is good for your brain. Experts recommend:
Monitoring the brain health of patients at risk of developing Lewy body dementia as early as possible is crucial to detect changes in function and enable early diagnosis, early intervention and treatment, and consequently, better health outcomes.
Additionally, individuals with modifiable Lewy body dementia risk factors, such as hypertension, diabetes, and depression, should closely monitor their brain health while modifying risk factors and making lifestyle changes.
Altoida’s mission is to accelerate and improve drug development, neurological disease research, and patient care. To learn more about our precision-neurology platform and app-based medical device, contact us!