The brain is arguably the most important organ in the human body. Brain health is an essential part of overall health and wellbeing—it is fundamental to our ability to think, learn, communicate, problem-solve, make decisions, respond to our environments, balance, move, and so much more.
Thanks to evolution, our brains have a robust defense system in place to protect against damage. The first layer of defense is the skull, which acts as armor to shield the brain from injury. Then comes the meninges, the three layers of the membranes that cover and protect the brain and spinal cord from contact with the skull. The final layer of protection is the cerebrospinal fluid.
Another crucial protective element is something called the blood-brain barrier. Below, we discuss the function of the blood-brain barrier and its dysfunction as it relates to neurological conditions.
The blood-brain barrier is a complex that surrounds most of the blood vessels in the brain. The primary function of the blood-brain barrier is to provide a protective barrier between the bloodstream and the extracellular space of the brain, allowing only certain substances, such as water, oxygen, and small lipid-soluble substances to cross from the blood into the brain. This critical function of the blood-brain barrier prevents toxins, pathogens, and other potentially dangerous substances from passing from the circulatory system into the brain.
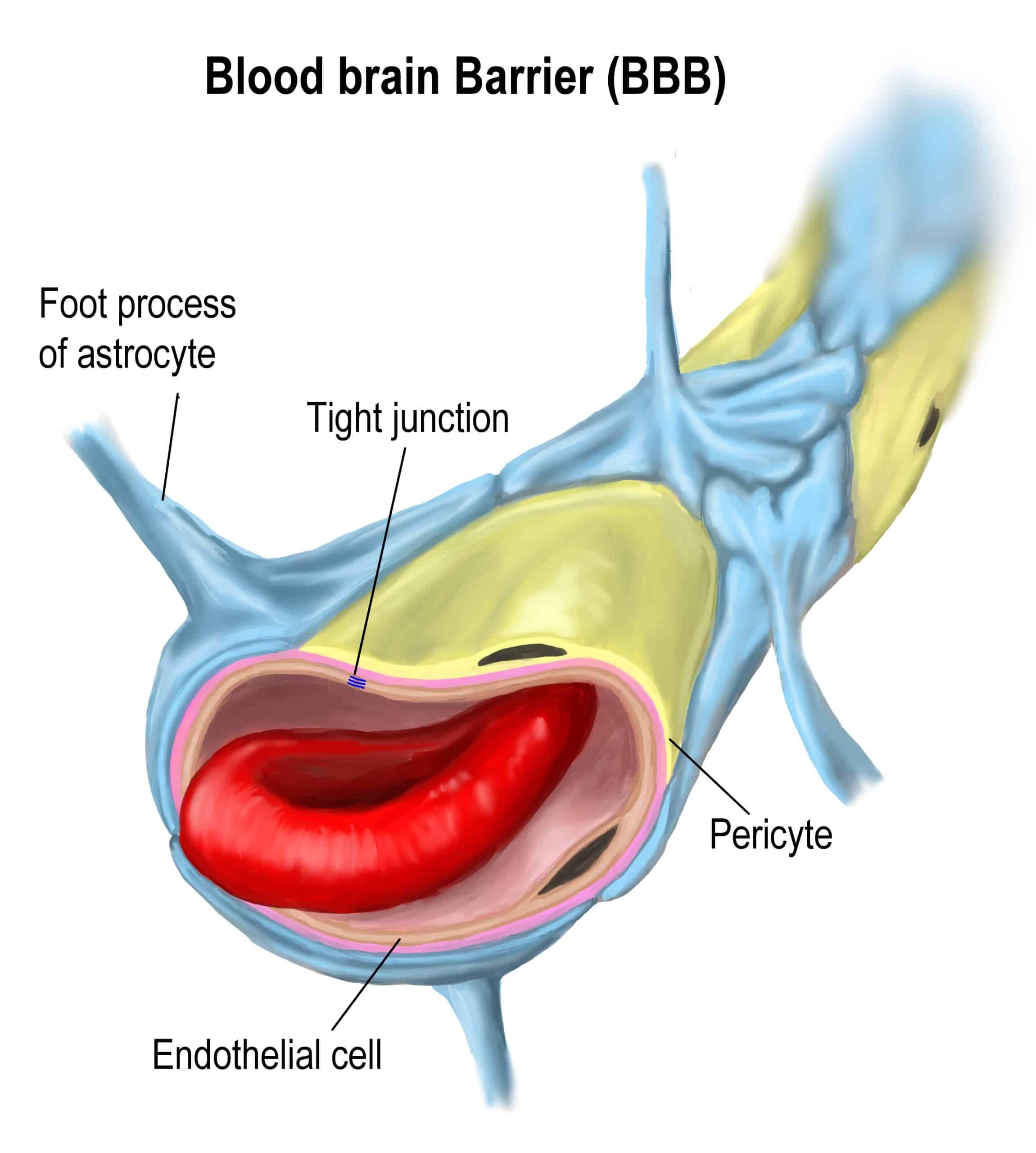
The blood-brain barrier follows the brain’s labyrinth of vasculature. It is composed of three cell types that communicate with one another to help form the blood-brain barrier and regulate its function and structure:
The central elements of its structure are the tight junctions of endothelial cells, the cells that line the interior surface of blood vessels. In other blood vessels throughout the body, there are small gaps between the endothelial cells, allowing small blood-borne substances to cross through these spaces and enter the surrounding tissues. The endothelial cells that make up the blood-brain barrier are different in that they are closely associated with one another, forming tight junctions that effectively restrict diffusion across the lining of blood vessels.
Pericytes are embedded in the vascular basement membrane and are physically connected to the endothelial cells in the brain through gap junctions and peg and socket arrangements. Pericytes help maintain and stabilize the monolayer of endothelial cells in the brain and are essential for the development of tight junctions.
Glial cells called astrocytes have astrocytic end-feet that extend to the walls of the blood vessels that are part of the blood-brain barrier. These cells play a key role in the maintenance and regulation of the barrier.
The blood-barrier barrier is a crucial immunological feature of the central nervous system—its integrity is vital for the maintenance of the very sensitive homeostasis of the central nervous system. The blood-brain barrier is effective in protecting the brain and spinal cord; however, like any protection system, it is not perfect and is subject to dysfunction.
When the permeability of this barrier increases, the function of the blood-brain barrier is disrupted. Inflammation, for example, can have a detrimental effect on the integrity of this barrier, making the barrier more permeable to immune cell infiltration.
This dysfunction can include changes to many different properties of the blood-brain barrier, including tight junctions, transporters, transcytosis, and leukocyte adhesion molecule expression. This breakdown can cause edema, altered signaling, disrupted ionic homeostasis, and immune filtration, which can, in turn, cause neuronal dysregulation and, ultimately, degeneration.
Dysfunction of the blood-brain barrier contributes to pathology in a range of neurological conditions, such as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, stroke, epilepsy, and traumatic brain injuries.
Alzheimer's disease and the consequent changes in the brain begin long before symptoms arise. An early blood-brain barrier breakdown and/or dysfunction has been shown in Alzheimer’s disease before the occurrence of dementia, neurodegeneration, and/or brain atrophy.
This emphasizes the importance of detecting Alzheimer's disease as early in the disease continuum as possible before irreversible damage has occurred to slow or even stop its progression. Early detection and early intervention are believed to offer the best chances of therapeutic success.
Altoida’s mission is to accelerate and improve drug development, neurological disease research, and patient care. To learn more about our precision-neurology platform and app-based medical device, contact us!